Understanding the Type 1 Diabetes Honeymoon Phase
The honeymoon phase in type 1 diabetes can be a confusing and often unexpected period following the initial diagnosis. It’s a time when the body still produces some insulin, leading to lower insulin requirements and potentially fewer fluctuations in blood sugar levels. While it offers a temporary reprieve, understanding the honeymoon phase is crucial for effective diabetes management. This phase varies significantly from person to person, making it essential to be aware of its characteristics and how to navigate its complexities. This involves recognizing the signs, adjusting treatment accordingly, and preparing for the eventual transition as the phase concludes. Managing expectations and maintaining a proactive approach is the key to a smoother transition.
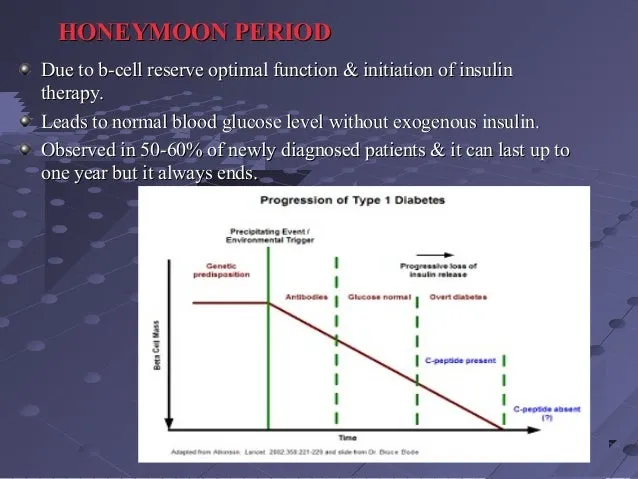
What is the Honeymoon Phase
The honeymoon phase, also known as the remission period, is a temporary phase that occurs after the initial diagnosis and treatment of type 1 diabetes. During this period, the pancreas still produces some insulin, though it is typically insufficient to meet the body’s needs. This residual insulin production can lead to reduced insulin requirements, fewer episodes of high or low blood sugar, and a feeling of improved health. The duration and intensity of the honeymoon phase vary significantly depending on factors such as age, initial blood sugar control, and the treatments initiated after diagnosis. This phase can be a welcome respite for newly diagnosed individuals, offering a chance to adjust to diabetes management before the disease progresses further.
How Long Does the Honeymoon Phase Last
The duration of the honeymoon phase varies greatly. It can last from a few weeks to several months, and in rare cases, even a year or longer. Several factors affect this duration, including the initial severity of the condition, the effectiveness of the treatment, and individual body responses. The intensity of this phase also changes over time, often with a gradual decrease in the amount of residual insulin produced by the pancreas. As the phase ends, the body’s ability to produce insulin diminishes further, and insulin needs gradually increase. Therefore, regular monitoring and adjusting insulin dosages are necessary to maintain good blood sugar control and prepare for the end of the honeymoon phase. The duration of the honeymoon period highlights the unique nature of diabetes management for each person.
Symptoms of the Honeymoon Phase
Recognizing the symptoms of the honeymoon phase can help in better diabetes management. During this period, individuals may experience reduced insulin requirements, fewer instances of high or low blood sugar, and an overall feeling of improved well-being. Some may also see a reduction in the symptoms they experienced before diagnosis, such as excessive thirst, frequent urination, and unexplained weight loss. These improvements can be deceptive, as the underlying autoimmune process continues to damage the insulin-producing cells in the pancreas. Therefore, it is essential to remain vigilant and continue regular blood sugar monitoring, even when feeling well, to avoid complications and ensure effective long-term diabetes management. Early recognition of these symptoms and an understanding of the changes happening in the body is critical.
Managing Insulin Dosage During the Honeymoon Phase
Adjusting insulin dosage is crucial during the honeymoon phase because of the fluctuating insulin production. Insulin needs often decrease during this phase, and maintaining the same insulin dosage as initially prescribed could lead to hypoglycemia, or low blood sugar. Regular monitoring of blood sugar levels is essential, often several times a day, to assess the impact of insulin and other diabetes management strategies. Adjustments should be made in consultation with a healthcare professional, considering factors such as diet, exercise, and overall health status. It is essential to remain proactive in managing insulin dosages to avoid health complications. Proper management provides a healthier life during and after the honeymoon phase.
Adjusting Insulin Based on Blood Sugar Levels
Insulin adjustments during the honeymoon phase should be based on consistent blood sugar monitoring. Keeping a detailed log of blood sugar readings, meal times, and insulin dosages helps identify patterns and the impact of insulin. Healthcare providers use this data to assess the effectiveness of current insulin regimens and make necessary changes. If blood sugar levels consistently run low, insulin doses need to be reduced. Conversely, if blood sugar levels remain high, then dosages may require adjustment. It’s crucial to remember that these adjustments are usually gradual, and it is important to avoid radical changes. Regular communication with a healthcare team ensures timely and appropriate adjustments that maintain optimal blood sugar control.
Monitoring Blood Sugar Levels Regularly
Regular blood sugar monitoring is fundamental to managing diabetes effectively, especially during the honeymoon phase. This involves checking blood sugar levels multiple times a day, often before meals, after meals, and at bedtime. The frequency of monitoring is typically determined by the healthcare provider, and it can be adjusted based on individual needs and blood sugar control. Monitoring helps detect high and low blood sugar levels, allowing for timely adjustments to insulin dosages, diet, and exercise. Using a continuous glucose monitor (CGM) can also provide a more comprehensive view of blood sugar trends, helping to identify patterns that may not be evident with finger-prick testing. Regular monitoring empowers people with diabetes to make informed decisions. This ensures they remain in a healthy state.
Adjusting Insulin Dosage
Making changes to insulin dosage during the honeymoon phase requires careful consideration and guidance from a healthcare provider. Insulin dosages should be adjusted incrementally based on blood sugar readings and other factors. A common approach is to adjust the basal insulin (long-acting) first and then fine-tune bolus insulin (short-acting) doses before meals. Factors such as carbohydrate intake, physical activity, and stress also need to be considered when adjusting insulin. The goal is to maintain blood sugar levels within the target range as much as possible, minimizing both high and low blood sugar episodes. Effective management involves continuous monitoring, diligent record-keeping, and regular communication with the diabetes healthcare team to personalize insulin adjustments and maintain optimal blood sugar control.
Diet and Exercise During the Honeymoon Phase
A balanced diet and regular exercise play a vital role in managing type 1 diabetes during the honeymoon phase. While insulin needs may be lower, maintaining healthy lifestyle habits is still critical for overall health and diabetes control. This combination helps to regulate blood sugar levels, improve insulin sensitivity, and reduce the risk of long-term complications. Consistent habits can significantly impact the management and outcome of the disease. This proactive approach helps to maintain healthy blood sugar levels, thereby improving overall health.
The Importance of a Balanced Diet
A balanced diet is crucial for managing blood sugar levels and maintaining overall health during the honeymoon phase. This involves focusing on whole foods, including fruits, vegetables, lean proteins, and whole grains. Controlling carbohydrate intake is key, as carbohydrates have the most significant impact on blood sugar levels. It is essential to monitor portion sizes, choose complex carbohydrates over simple sugars, and spread carbohydrate intake evenly throughout the day. Working with a registered dietitian can provide personalized meal plans and guidance on making healthy food choices. Staying consistent with the plan helps maintain stable blood sugar levels, improving the management of the condition. Proper diet helps prevent complications.
Exercise and Its Impact
Regular exercise is beneficial for individuals with type 1 diabetes during the honeymoon phase. Exercise improves insulin sensitivity, which means the body can use insulin more effectively, helping to lower blood sugar levels. Physical activity also helps with weight management, cardiovascular health, and overall well-being. It is essential to discuss an exercise plan with a healthcare provider, as exercise can affect blood sugar levels. Before, during, and after exercise, regular blood sugar monitoring is crucial. It is also important to understand the impact of exercise, and proper measures should be taken to avoid low blood sugar episodes. Consistency is key to maintaining optimal blood sugar control and overall health during this phase. Proper exercise helps patients lead healthy lives.
Emotional and Psychological Aspects

Living with type 1 diabetes and navigating the honeymoon phase can have emotional and psychological impacts. The initial diagnosis itself can bring feelings of shock, sadness, and anxiety. The fluctuating nature of blood sugar levels and the need for constant monitoring can lead to stress and frustration. During the honeymoon phase, the temporary improvement in blood sugar control can also lead to feelings of relief, but the eventual transition to increased insulin needs can cause disappointment and fear. This understanding of the emotional aspect is essential for comprehensive diabetes management. Seeking support, education, and coping strategies can help individuals navigate the emotional challenges associated with this phase.
Coping with Emotional Changes
Coping with emotional changes during the honeymoon phase involves several strategies. It includes acknowledging and accepting the emotions, such as sadness, anxiety, and frustration, that arise. Practicing self-care activities, such as relaxation techniques, exercise, and hobbies, can help manage stress. It is crucial to develop coping mechanisms, like journaling or mindfulness, and to communicate openly with healthcare providers. Learning to adapt and manage the illness is essential for both mental and physical health. Creating a positive support system through family, friends, and other individuals can significantly improve the ability to cope with the emotional challenges. Taking control of emotions makes diabetes management more manageable.
Seeking Support and Education
Seeking support and education is crucial for managing the emotional and practical challenges of the honeymoon phase. Joining a diabetes support group provides a space to connect with others who understand the complexities of the disease and share experiences and advice. Education about diabetes management, including insulin adjustments, diet, and exercise, is essential. Healthcare professionals, diabetes educators, and mental health professionals can provide valuable support and guidance. Engaging with reliable online resources, educational materials, and attending workshops can help individuals and their families gain valuable knowledge and strategies to cope with diabetes. By seeking education and building a support network, one can find comfort. This knowledge empowers individuals to manage the condition effectively.
Long-Term Management and Transition

The honeymoon phase is a temporary period, and the focus shifts to preparing for the eventual transition. Understanding the expected decline in insulin production and adjusting to changing insulin needs is crucial for ongoing management. Adopting a proactive approach to long-term diabetes care helps individuals maintain good blood sugar control and prevent complications. This involves regular check-ups, continuous education, and adapting to changing needs. The transition to the next phase requires a shift in mindset, from relying on the temporary benefits of the honeymoon phase to a long-term perspective of continuous diabetes management. It is essential to plan for the future to stay healthy.
Preparing for the Post-Honeymoon Phase
Preparing for the post-honeymoon phase involves several key strategies. Understanding that insulin needs will increase over time is crucial, and it is essential to anticipate adjustments. It is important to continue to monitor blood sugar levels regularly, monitor eating habits, and adjust insulin dosages. Regular check-ups with a diabetes healthcare team can help identify changing needs and implement strategies. Education about the long-term aspects of diabetes management is essential, including potential complications and how to prevent them. Proactive planning and a comprehensive understanding of the condition help make the transition smoother, ensuring continued diabetes management. Regular reviews help to maintain health and anticipate any further steps to take.
Continuing to Manage Diabetes Effectively
Continuing to manage diabetes effectively involves adopting a holistic approach. This includes: adhering to a balanced diet, maintaining an active lifestyle, and regularly monitoring blood sugar levels. It is also essential to take insulin as prescribed and to schedule routine appointments with healthcare providers. Participating in ongoing diabetes education, seeking support from family and friends, and staying informed about new developments in diabetes care are also critical. It also includes making adjustments to lifestyle and other health practices to maintain optimal health. Consistent management helps to live a healthy life while living with diabetes.
